Introduction
Welcome to Sport And Spine Physiotherapy’s Patient Guide for Parkinson’s Disease Rehabilitation.

This guide will help you understand:
- how Parkinson’s Disease develops
- how Parkinson’s Disease affects the body
- rehabilitation for Parkinson’s Disease consists of
- research related to Parkinson’s Disease
Anatomy
What is Parkinson’s Disease?
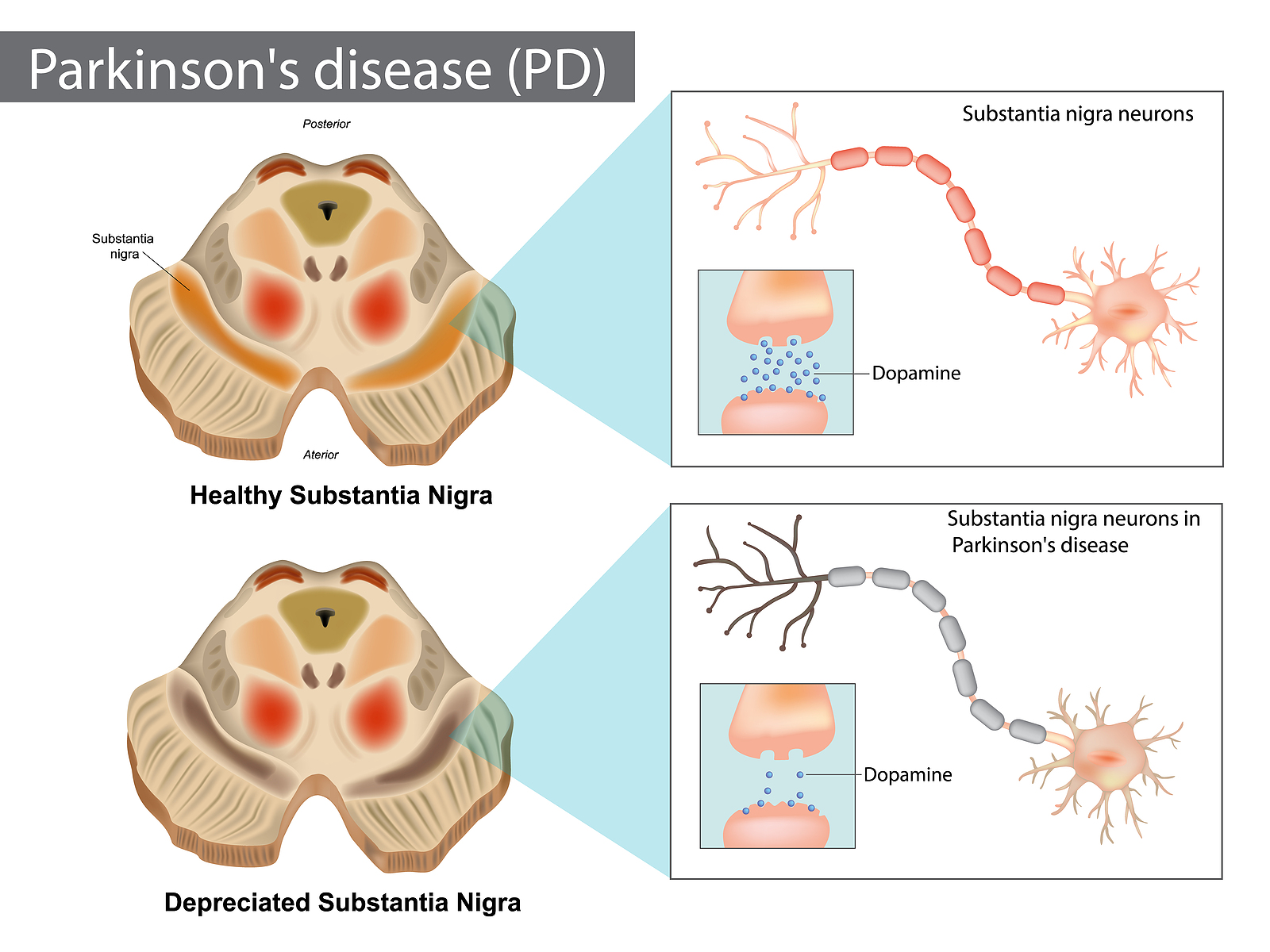
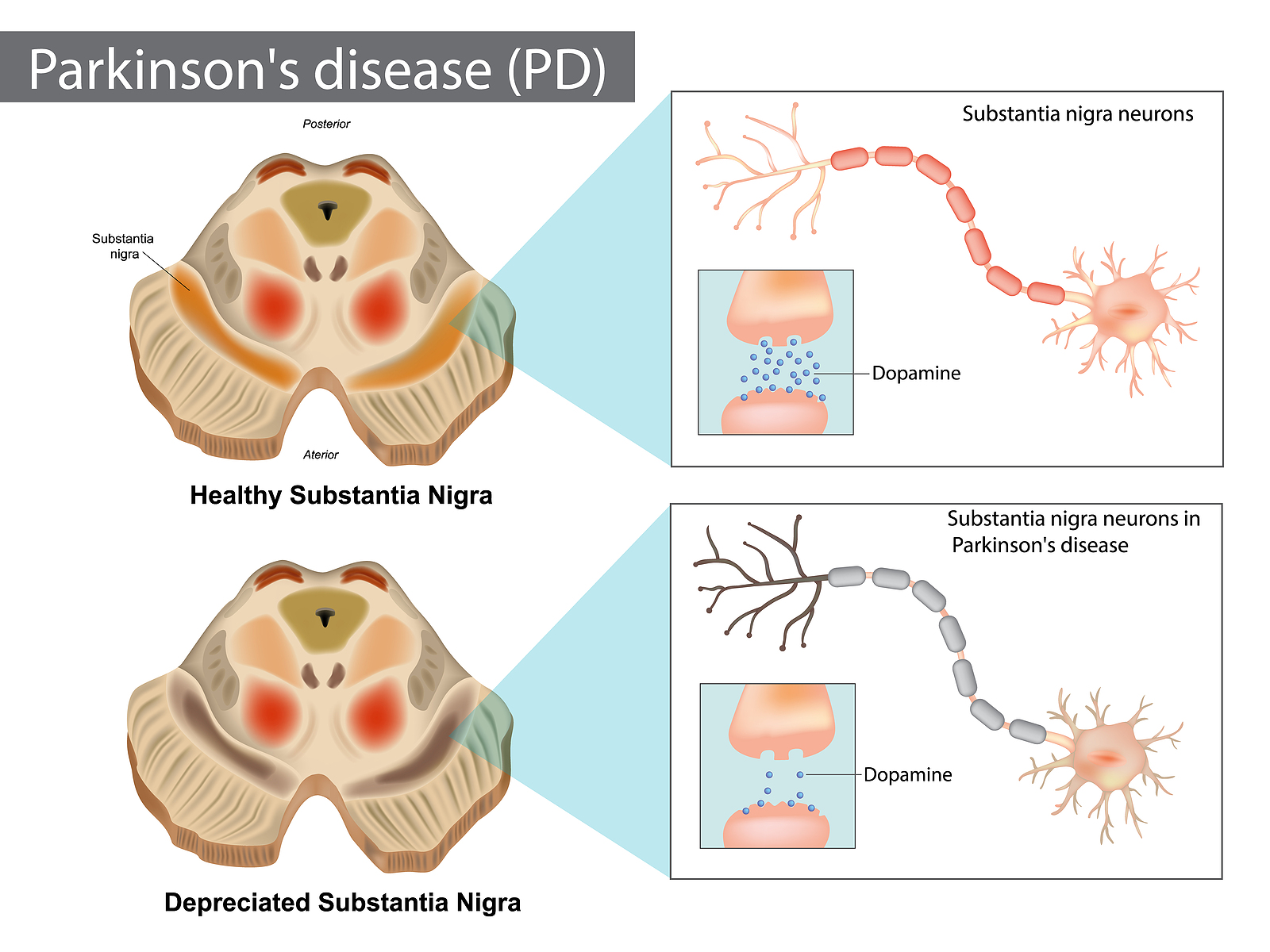
Parkinson’s Disease—also known as Parkinson’s or PD—is a progressive neurodegenerative disorder that affects the nervous system. This condition develops when nerve cells (neurons) in a structure called the substantia nigra become impaired or die. The substantia nigra belongs to a group of midbrain structures called the basal ganglia. Under healthy states, nerve cells in this region produce a neurotransmitter (chemical messenger) called dopamine. This neurotransmitter helps regulate mood, memory, motivation, and coordination.
When substantia nigra nerve cells become impaired or begin to die, they gradually stop producing dopamine, which leads to physical symptoms such as uncontrollable shaking, balance and coordination issues, and stiffness. Mental and behavioral changes, memory problems, sleep disturbances, fatigue, and depression may also develop. Symptoms typically begin to appear gradually and slowly worsen over time. The reason why nerve cells stop producing is unknown, but certain risk factors a system in the midbrain (substanstia nigra) which produces the chemical called dopamine, stops producing this chemical. It is still unknown why the cells stop producing dopamine. The chemical dopamine is required in the body for many things including coordination, mood, memory and motivation. It is interesting to note that usually by the time someone is diagnosed with Parkinson’s disease, around half of the dopamine-producing cells have already died.
History of Parkinson's Disease
James Parkinson, a British apothecary, was credited with providing the first publication about this disease in 1817. He reported a summary of six cases of what he called ‘shaking palsy’ or ‘paralysis agitans’. All six patients presented with similar symptoms such as tremors, stooped posturing, abnormal gait, paralysis, and diminished muscle strength.
Additional researchers, including Jean-Martin Charcot, continued to study the disease, which led to the expansion of the early description. Charcot’s contribution also distinguished Parkinson’s disease from multiple sclerosis. By the end of the 20th century, a great advancement in the discovery of a genetic component that occurs in some people with the disease was made.
In particular, the early onset of Parkinson’s is often inherited, and certain forms of this disease are linked to specific gene mutations. For one Italian family—in which five generations were studied—it was discovered that over 60 family members were diagnosed with Parkinson’s disease. To better understand the factors that lead to Parkinson’s, an abundance of research is ongoing throughout the 21st century.
Signs and Symptoms
The type and severity of symptoms a person with Parkinson’s may display differs for each individual. In most cases, symptoms that occur early on are subtle and progress gradually. For some individuals, mild tremors may develop or they may struggle to get out of a chair. Others may notice that their handwriting has changed or experience a frail voice when they are speaking.
Family members and friends may also be the first ones to notice small changes in an individual who has early Parkinson’s disease. For instance, they may observe blank, emotionless facial expressions from their loved one, or that the person is struggling to move there is no single symptom that determines that one has PD. Nor is there one single test that is used to delineate that you have the disease. Each individual who is diagnosed with Parkinson’s disease may exhibit distinct signs and symptoms. A series of tests usually need to be performed to confirm suspected cases of Parkinson’s. However, the most common signs and symptoms are:
- muscle tremors in the hands, arms, head, jaw, or legs
- postural instability and impaired balance (difficulty remaining upright, especially when standing still or getting up from a chair)
- difficulty walking, taking small rapid steps (festinating gait)
- with walking, often taking shuffling (festinating) steps,
- slowness of movements and speed (bradykinesia)
- delayed ability to perform desired movements (akinesia)
- twisting or repetitive movements due to involuntary muscle contractions (dystonia)
- tense, stiff muscles that limit movement (rigidity)
- stooped posture or postural instability (body is often bent forward)
- increased postural sway (bodily motion when standing still)
- sleep disturbances and sudden movements during sleep
- loss of automatic movements such as blinking or swinging arms when walking
- decline in automatic facial expressions (facial masking)
- problems projecting one’s voice (only able to speak softly)
- handwriting changes (may become too difficult to coordinate) and/or can become very small (micrographia)
- psychotic episodes (seeing, hearing, smelling items that are not real)
- loss of motivation
- frequent dizziness
- fatigue
- drooling
- loss of smell
- constipation
- depression
Risk Factors
There are several factors that appear to play a role in the development of PD: There are several factors that appear to play a role in the development of PD:
- Age: The biggest risk factor for developing Parkinson’s disease is advancing age. Most commonly people are diagnosed with PD around the age of 60 or older. However, the risk of getting Parkinson’s disease increases with age and is considerably higher by the time an individual reaches the age of 85. Although it is uncommon for people to be diagnosed with this disease before the age of 60, it does occur. This type of case is referred to as ‘young-onset Parkinson’s disease’.
- Sex/Gender: Research has consistently demonstrated that men are more frequently diagnosed with Parkinson’s disease than women.
- Heredity: Having one or two close relatives with Parkinson’s disease increases the chances of developing this condition. However, this risk remains low unless many members of the same family have Parkinson’s.
About 10-25% of people diagnosed with this disease have a genetic link, while the majority of people with Parkinson’s disease did not inherit the condition.
In addition, there are some genetic variations (mutations) that can increase the chance of developing Parkinson’s, but people who have these mutations do not always develop this disease. Ongoing research is focusing on genetics as a causative factor for the disease. .
- Environmental Factors: Some environmental factors such as pollution, circulating viruses, heavy metals, pesticides, herbicides, illicit drugs, and exposure to additional toxins may play a role in the onset of Parkinson’s disease.
- Head trauma: There is some evidence that suggests a history of traumatic brain injury (TBI) or repeated head trauma (e.g., boxers) may increase the risk of developing Parkinson’s disease. A serious brain injury can lead to the accumulation of a harmful protein called alpha-synuclein that causes nerve cell deterioration and death. Elevated levels of alpha-synuclein in nerve cells and cerebrospinal fluid (CSF) are associated with the onset of Parkinson’s for some individuals.
- Ethnicity: Research regarding the ethnicity-related risk of acquiring Parkinson’s is ongoing, but most studies show that White populations generally have the highest prevalence of Parkinson’s disease. However, individuals of Hispanic or Black ethnicity who are diagnosed with this condition often have a higher risk of experiencing severe cognitive impairment
Diagnosis
How do healthcare providers diagnose Parkinson's Disease?
To date, there is no single test that can accurately identify the presence of Parkinson’s disease. Instead, the diagnostic procedure involves assessing medical history, presenting symptoms, neurological tests, and a physical examination that a healthcare professional conducts.
Although Parkinson’s disease is often diagnosed when the classic motor (movement) signs or symptoms are present such as tremors, muscle rigidity, balance issues, festinating gait, or difficulty moving, current research points to the identification of non-motor signs. More specifically, signs such as the loss of smell, dizziness, constipation, sleep disturbances, and depression often become evident ahead of the motor-related signs and can potentially be used for earlier diagnosis of the disease in the future.
If a healthcare professional suspects Parkinson’s disease, the next step is a referral to a doctor who specializes in neurological disorders, such as a neurologist.
Examinations
A combination of physical, neurological, and imaging examinations may be necessary to rule out the possibility of other neurological diseases that may cause symptoms similar to Parkinson’s disease. The physical exam includes a visual assessment, palpation (feeling limbs and muscles), percussion (tapping body parts to produce sound), and auscultation (using a stethoscope). During a neurological exam, an individual may be asked to walk, sit, stand, and move the limbs in specific ways to evaluate coordination and balance. Memory, sensory function, and reflexes may also be assessed.
In addition, imaging tests such as magnetic resonance imaging (MRI), positron emission tomography (PET) scan, or an ultrasound may be performed. A specialized single-photon emission computerized tomography (SPECT) scan called a dopamine transporter scan (DaTscan) is an alternative imaging exam, but it is expensive and not performed routinely.
The final diagnosis depends on the cumulation of results from the series of tests that are conducted.
Medication
There are many drugs that are being used to treat the PD physiological disease process as well as many drugs that are used to treat the symptoms that the disease brings with it. Unfortunately, no drug is currently available that reverses the effects of Parkinson’s or stops the disease from progressing.
Initial drug treatment typically aims to restore and mimic the effects of dopamine, or to stop the breakdown of dopamine in the brain. Some doctors often recommend a trial period of a dopamine-type medication such as levodopa to see if it is effective at decreasing symptoms (e.g., tremors, motor difficulties). Levodopa, which is an amino acid the body converts into dopamine, became the primary agent to treat the symptoms of Parkinson’s disease during the early 1900s.
Furthermore, a positive response to levodopa was an indication or confirmation of Parkinson’s disease, and due to its effectiveness it was once considered the gold standard for Parkinson’s management. In some cases, levodopa is still the first line of treatment due to its function as a dopamine replacement agent.
However, levodopa requires 2-3 weeks to initially take effect, and it has a short half-life of about 90 minutes, which means the body rapidly breaks it down. As the medication’s effects wear off, the symptoms may start up again until another dose of levodopa is taken. In addition, levodopa may cause dyskinesia (uncontrollable fidgeting) as the levels of dopamine start to increase in response to taking this drug, especially in individuals with young-onset Parkinson’s disease. This drug also loses its effectiveness over time.
To combat these types of issues, levodopa may also be combined with another medication called carbidopa to form Sinemet (carbidopa-levodopa), which helps the drug cross into the brain. The combination of these two drugs also offers extended-time release that improves its effectiveness.
As a result, Sinemet is now referred to as the gold standard in Parkinson’s treatment in comparison to other drugs that mimic dopamine in the brain (dopamine-agonists) or those that stop the breakdown of dopamine, such as monoamine oxidase B (MAO-B) inhibitors, catechol-O-methyl transferase (COMT) inhibitors, and anticholinergics.
A doctor will evaluate the most up-to-date and effective medications for each individual case. The medication that is recommended also depends on the presenting symptoms, an individual’s age, overall physical health, lifestyle, and whether the symptoms affect activities of daily living such as maintaining balance, walking, and using the hands properly.
Unfortunately, some of the medications that are used to treat Parkinson’s disease can cause or worsen certain symptoms (e.g., dyskinesia) as the dosage is increased. It is important to note that dyskinesia is not a symptom of Parkinson’s, but rather a side effect that is caused by some medications. Many patients choose to continue taking medication despite the occurrence of dyskinesia because without the medication their other symptoms worsen, making it difficult to manage their daily lives.
Rehabilitation
Participating in a rehabilitation program is a very important part of living with Parkinson’s disease. The goal of rehabilitation is not to reverse the effects of Parkinson’s—as this is not always possible—but rather to slow down the degenerating effects of the disease. Rehabilitation helps target symptoms and maximizes the ability to function efficiently despite symptoms. Your physiotherapist typically aims to keep an individual as independent as possible for as long as possible. There may also be specific lifestyle goals that a physiotherapist can help with.

Regular exercise is important for everyone, but research shows that exercise is particularly effective for people living with Parkinson’s, as it can affect how well dopamine is used in the brain.
Every Parkinson’s disease journey is different, so a physiotherapist will focus on developing an individualized exercise program that minimizes specific symptoms (e.g., tremors, stability issues, writing difficulties). Exercise for people with Parkinson’s may also include a combination of exercises for strength, balance, endurance, flexibility, and coordination. Several exercise techniques may be used by your physiotherapist to establish a therapeutic regimen.
Therapeutic Exercises
Cardiovascular (aerobic) exercise:
Several studies have shown the benefits of high-intensity exercise, as this type of activity slows the general aging of the brain in healthy adults. High-intensity exercise is defined as exercise that raises the heart rate and promotes deeper breathing. In people with Parkinson’s, high-intensity aerobic exercise also helps slow down motor skill degeneration, protects against depression, and improves quality of life.
Your physiotherapist can recommend what type of high-intensity exercise might be the most beneficial, the degree to which it should be performed, and how often to exercise. The consensus is that the more cardiovascular exercise an individual performs, the better! This means that even small amounts of exercise count!
As a guide, one study showed that about 2.5 hours of physical activity each week slowed the decline in quality of life in people living with Parkinson’s disease. It is helpful to choose a form of exercise that is enjoyable, and consistency is the key. Enhanced benefits have been observed with exercise programs that are six months or longer in comparison to programs that only last for a few weeks or months.
Strength training: Using weights can also be beneficial in improving strength, particularly lower body strength—an important aspect of health that has a direct effect on the ability to maintain balance. In addition, both upper and lower body strength training has been shown to help decrease slowness of movement (bradykinesia), which may be a symptom for some people with Parkinson’s. In addition, strength training can improve the ability to move more easily and perform regular daily activities.
Balance, posture, and fall prevention: The loss of healthy dopamine levels affects the ability to initiate or make continuous movements. Sometimes it is difficult for people with Parkinson’s disease to start a movement (akinesia), or movements are slow (bradykinesia). Furthermore, movements that are normally automatic are also affected, such as blinking, swallowing, walking while talking, or arm swinging with walking. Individuals with Parkinson’s may also have to be reminded to continue these types of movements.
A change in the ability to initiate movements or having slower and fewer automatic movements can directly affect posture and balance. This can in turn increase the risk of falling. It has been well proven that balance can improve with training! For this reason, a physiotherapist will work on posture and balance exercises. Your physiotherapist will also discuss strategies that make regular activities less risky for falls and the home environment safer.
Movement strategy training: Different types of movement training can assist with maintaining regular motion and regulating automatic movements. Therefore, your physiotherapist may work on reciprocal training, which aims at reintegrating normal reciprocal movements such as arm swinging and trunk rotation with walking. It has also been shown that training with oversized movements, such as exaggerated arm or leg swings or taking extra-large steps when practicing, can help maintain smaller, similar movements that are normal with everyday activities. Your physiotherapist may also actively train an individual with Parkinson’s through activities that involve performing two tasks at once (dual-task training), such as walking and carrying a cup of water, walking and talking, or walking while doing mental tasks. Using mental imagery to imagine the appropriate movement may also be used to assist the rehabilitation process.
Additional Activities: Additional activities such as dancing, non-contact boxing, tai chi, qi-gong, biking, and yoga have all been shown to help target symptoms of Parkinson’s disease. As a result, a physiotherapist may incorporate these types of activities into the exercise routine. In addition, your physiotherapist may encourage participation in group exercise or a support group. It is well proven that group activities can positively benefit overall well-being. This is also true for people with Parkinson’s.
Interdisciplinary Team Therapy
Physiotherapists may recommend working with other healthcare professionals to better address specific rehabilitation needs. For instance, they may suggest speaking with an occupational therapist (OT) who can focus on fine motor tasks required for daily living activities such as getting dressed, bathing or showering, writing, cooking, and any other activities an individual may be struggling with. They can also assist with advice regarding home modifications that can help reduce fall risks or provide support to foster independence.
Your physiotherapist may also suggest a consultation with a speech-language pathologist (SLP) to address symptoms such as poor voice projection, speech difficulties, swallowing concerns, diminishing facial expressions, or communication problems.
Research regarding additional therapeutic exercises, training techniques, and rehabilitation methods that may benefit individuals with Parkinson’s disease is ongoing.
Current Research
The medical community’s understanding of Parkinson’s disease is increasing daily. Continuous, extensive, and ongoing research seeks to elucidate more information about factors that contribute to the onset and progression of Parkinson’s to improve diagnosis accuracy, to facilitate earlier diagnoses, and to provide more effective treatments. Current research is focusing on:
Biological markers: Finding biological markers that can help identify individuals at risk for developing Parkinson’s disease early on is an important area of focus. Currently, by the time individuals have developed symptoms of Parkinson’s that lead to a diagnosis, it is believed that a 40-50% decline in dopamine levels has already occurred. Some reports suggest that the percentage may be even higher.
Alpha-synuclein: Studying mutations in the alpha-synuclein proteins and other molecules in the brain that are involved in the transmission of signals is another key area of research. Studies have previously shown that, in people with Parkinson’s, alpha-synuclein proteins mutate and aggregate into clumps called Lewy bodies. Research is ongoing to discover ways to prevent this mutation and clumping, as well as potential ways to vaccinate against this mutation.
Cellular processes: Additional studies are looking into the cellular processes of mitochondria (the power producers in our cells), which seem to be affected by Parkinson’s disease. The role of oxygen levels, gut bacteria in alpha-synuclein buildup, and abnormal inflammatory responses in the loss of dopamine production and the progression of Parkinson’s disease are also under investigation.
It is important to note that several cellular processes that are involved in the development of Parkinson’s disease are related to the occurrence of other neurodegenerative diseases, such as Alzheimer’s disease, amyotrophic lateral sclerosis (ALS), and Lewy body dementia, which along with progressive dementia, presents with Parkinson’s physical symptoms.
Genetics and Pharmacology: Research is currently underway to identify any potential genetic precursors or mutations that may contribute to the development of Parkinson’s disease. Similarly, pharmacological research is continually being conducted to determine the best types of medications to combat the degenerative process of Parkinson’s as well as the presenting symptoms. Certain medications that have been approved for use in other diseases are being tested for Parkinson’s disease treatment. Brand new drugs are also being developed in response to novel research results. In addition, clinical trials involving surgically implanted drug pumps are currently underway to develop a more effective delivery method for Parkinson’s disease medications. This method can help prevent the ‘wearing-off’ effect of traditional prescriptions.
Environmental Risk Factors and Toxins: Research continues to evaluate the potential effects of environmental risk factors in the development of Parkinson’s disease, including pollution, exposure to toxins, or circulating viruses. Currently, researchers are focusing on several clusters of patients worldwide who live in the same environment and have subsequently developed Parkinson’s. Interestingly, the majority of these cases involve young-onset Parkinson’s disease.
Motor Patterns: Parkinson’s disease seriously affects normal movement (motor) patterns. Individuals with this condition may experience the inability to move when they desire (akinesia), slowness of movement (bradykinesia), or may develop abhorrent movements (dyskinesias) while taking medication.
Current research is focusing on why these movements occur and how best to treat all types of movement patterns to minimize the negative effect motor issues have on people’s everyday lives.
Deep Brain Stimulation: Deep brain stimulation can be used in advanced Parkinson’s disease and is generally recommended when medications have failed to help. With deep brain stimulation, electrodes are surgically implanted into the brain and stimulated to help treat symptoms of Parkinson’s (e.g., tremors, gait issues, balance difficulties, memory problems). Researchers are investigating the specific areas that need to be targeted, how much stimulation is required, and how often stimulation should be applied.
Exercise: Exercise is a well-proven strategy that helps modify Parkinson’s disease symptoms. Regular exercise also helps prevent symptoms from rapidly getting worse. Ongoing research is focusing on which types of exercises are most beneficial and the length of time and duration that affords the most benefits.
Overall, many researchers agree that because Parkinson’s disease appears to develop due to a combination of genetic (e.g., gene mutations) and environmental factors (e.g., toxin exposure), research and treatment should focus on broadening the range of bodily systems that are targeted in people with Parkinson’s.
Sport And Spine Physiotherapy provides services for physiotherapy in Sarnia.
Conclusion
Physiotherapy services at Sport And Spine Physiotherapy can help you manage your Parkinson’s Disease.
Our highly skilled physiotherapists can help maximize your functional potential and delay any physical declines as long as possible. Starting physiotherapy during the early stages of Parkinson’s helps to improve outcomes, so it is important not to delay a consultation.
Portions of this document copyright MMG, LLC.